People with addiction are at risk of premature death. Defining terms and making sure we know what we’re talking about is an imperative.
Illogic and misinformation can kill people with addiction.
Do no harm.
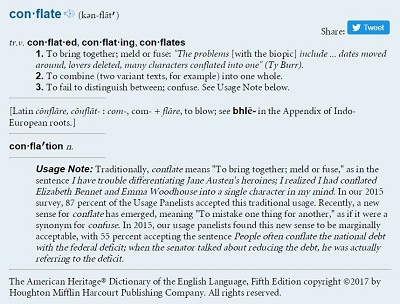
Discussion of addiction is plagued with conflation, i.e. thinking things are the same when they are different. Discussion is also compromised by confusing correlation with causation, i.e. assuming that if things happen at the same time, one caused the other.
 Following is a list of terms and basic definitions used in this guide. Terms are in narrative order, not in alphabetical order. Terms explicitly not used are listed at the foot of this post.
Following is a list of terms and basic definitions used in this guide. Terms are in narrative order, not in alphabetical order. Terms explicitly not used are listed at the foot of this post.
Addiction is the generally-used, non-clinical term for substance use disorder.
A substance use disorder is a medical condition involving the organ of the brain. The primary symptom of the disorder is persistence in behavior despite negative consequences. (For brevity and the general audience intended for this guide, “addiction” is the term used most often, but interchangeably with “substance use disorder.”)
Dependence is conflated with addiction. The difference between addiction and dependence can mean life or death. Dependence exists when a substance is needed to function and physical withdrawal symptoms will result without the substance. Humans are dependent upon the substances of water and air to function and experience physical symptoms without them. People who cease taking antidepressants can experience withdrawal symptoms. People who cease taking blood pressure medication can experience withdrawal symptoms. People who do not persist in negative consequences, but experience withdrawal symptoms when ceasing substances, are dependent upon those substances, but not addicted to them.
Similarly, babies born to mothers dependent on substances – whether opioids, antidepressants, nicotine or others – may experience withdrawal symptoms, but are not born addicted to those substances. Babies are developmentally incapable of persisting in behavior despite harmful consequences.
Making it through withdrawal from substance dependence is not a treatment nor a cure for addiction.
The neuroscience of addiction suggests that through compromising the brain’s basal ganglia, extended amygdala, and prefrontal cortex, addiction under-sensitizes people to pleasure, over-sensitizes them to pain, automates use of the substance to feel, not necessarily good, but normal, weakens decision-making abilities, magnifies emotional highs and lows and incapacitates the ability to regulate them, interferes with recognizing cause-and-effect relationships, and confounds the ability to make a plan and follow through with it.
Co-occurring disorders are medical – including physical illnesses and substance use disorders – and mental illnesses, that may occur simultaneously in an individual. The medical condition of substance use disorder may co-occur with mental illnesses such as anxiety, mood, thought, and/or personality disorders, and/or physical illnesses.
Determining which symptoms go with which disorder, how to manage symptoms, and treat the conditions, is an on-going conundrum. Which are due to brain malfunctions, cognitive distortions, perhaps unregulated emotions?
Further, the definition of addiction is conflated with the symptoms of the illness. Although some people with substance use disorder may engage in behaviors that are perceived by society to be immoral, criminal, or illogical, behavior related to addiction results from brain functioning, not from moral functioning, and persists despite negative consequences. Ergo, moral or religious instruction would not be a treatment for a brain disorder. Counseling might help a person with substance use disorder manage symptoms of the illness, but would not directly treat the brain for a brain condition.
Evidence-based treatment is what research reports works for most people, most of the time, better than other treatments, and better than no treatment. Specifically, that means the treatment is supported by numerous, peer-reviewed scientific experiments with rigorous methods that include control groups, randomization of subjects to experimental conditions, and bias-free samples, with statistically significant results. Some treatments that are evidence-based to work for groups may not be helpful to a particular individual, however. It is imperative that individuals and their treatment teams continually co-monitor current condition and progress.
Anecdotal data is an individual’s personal experience. Research data – the evidence resulting from research experiments – is conflated with “anecdotal data.” Data from a sample size of one does not provide sufficient information from which a generalization can be made about a group or population. Principles believed to account for outcomes from inspirational individual stories, practitioner wisdom, or theories based on logic, cannot be safely applied to others without first subjecting those principles to rigorous research.
Medical care is the first line of treatment recommended by the medical professionals and researchers who authored Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health. Medications approved by the FDA for treating substance use disorder are listed here. Currently, no licensed treatments are available for stimulant use disorder.
As long as addiction is attributed to some aspect of the person – lack of motivation, un-readiness for change, lack of self-restraint while self-pleasuring, willful criminality – the myth of addiction as a moral problem within the person’s power to correct, rather than a medical problem in need of medical care, is perpetuated.
Terms not used in this guide:
Addict and alcoholic. The complexity of human identities defies the limits of definition by trait or condition. This guide, as does the new edition of the Associated Press style manual, uses the terms “person with addiction” and “person with alcoholism.”
Substance abuse. “Abuse” means to wrongly maltreat. “Self-abuse” is a pejorative term for masturbation. “Sexual abuse” and “child abuse” are heinous acts. Use of the term “substance abuse” conflates addiction with sexual acts and violation, misrepresents the medical illness of addiction, perpetuates stigma, and needs to be jettisoned from any reference to addiction.
Disease. Although carefully defined by NIDA, the term “disease” used to explain addiction can be unhelpfully misunderstood by laypeople. Scientists and researchers may eventually decide other terms may be more accurate. Terms used in this guide include “disorder,” “condition,” and “illness.”
Dopamine. The neurotransmitter dopamine is conflated with “pleasure.” But dopaminergic pathways involve reward-related cognitions that include incentive salience (desire or “wanting”), pleasure (“liking”), and positive reinforcement, i.e. a desired event occurs. Most laypeople are not qualified to discuss addiction at this level. Addiction is more complicated than simply stating, “It’s all about dopamine.”
Enabling, codependency, “hit bottom,” and “tough love.” People with medical illnesses that can result in premature death need care, support, and treatment, especially when their symptoms are severe and life-threatening. For further reading:
- Why the Codependcy Myth of Addiction Needs to Die
- Tough Love and Addiction: Why It Doesn’t Work
- The Tragic, Pseudoscientific Practice of Forcing Addicts to Hit ‘Rock Bottom’
- What You Really Don’t Know About Recovery
Trading one addiction for another. Use of substances, for any reason, prescribed or not, where behavior does not persist despite negative consequences is not addiction. Opioid replacement therapy does not replace one addiction with another.
. . . . .
“A substance use disorder is a medical illness characterized by clinically significant impairments in health, social function, and voluntary control over substance use.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 4-1
“Addiction is a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences.”
– National Institute on Drug Abuse (NIDA), a division of the National Institutes of Health (NIH), 2014
“Research has shown that substance use disorders are similar in course, management, and outcome to other chronic illnesses, such as hypertension, diabetes, and asthma.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 1-18
“Remission of substance use and even full recovery can now be achieved if evidence based care is provided for adequate periods of time, by properly trained health care professionals, and augmented by supportive monitoring, RSS [recovery support services], and social services.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 1-19
“People suffering from addictions are not morally weak; they suffer a disease that has compromised something that the rest of us take for granted: the ability to exert will and follow through with it.”
– Nora Volkow, M.D., Director of NIDA, 2015
“Be suspicious if someone is calling you a ‘client’ when seeking help. Addiction is a disease, best treated by a physician who treats ‘patients’ w/ medical & mental diagnoses or knows where to refer for evidence based care.”
– Molly Rutherford, M.D., via Twitter, 12/28/17
“Unfortunately, despite decades of research, it cannot be concluded that general group counseling is reliably effective in reducing substance use or related problems.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 4-26
“Do not attempt to take away a person’s main means of trying to cope with pain and suffering until you have another effective coping strategy in place.”
– Alan Marlatt, Ph.D., 2004
“If you believe that something is essential to your survival, your priorities won’t make sense to others.”
– Maia Szalavitz, 2016
“”You have to think complexly about complex things.””
– Robert M. Sapolsky, Ph.D., 2017
“People may not have caused their own problems but they have to solve them anyway.”
– Marsha Linehan, Ph.D., 2014
“Love, evidence & respect.”
– Maia Szalavitz’s answer via Twitter to the question, “What fights addiction?”, 6/25/16
“Deciding to use substances like tobacco, alcohol, marijuana or heroin does not make people less human. It reflects the fact that they are human.”
– Hakique Virani, M.D., People use drugs, get over it, CBC Radio-Canada, 2017
“Try to treat other people as if they possessed precious hearts and infinite souls. Everything else will follow.”
– David Brooks, Op-Ed columnist for The New York Times, 1/18/18
“It’s my life. Don’t you forget.”
– “Talk, Talk,” The Music Machine
This post is part of a series on evidence-informed self-care for addiction. Self-care is NOT an evidence-based treatment for addiction. However, when treatment is scarce or denied, people with addiction must take treatment matters into their own hands. The table of contents is here and posts are published in the category entitled Guide.
The views expressed are mine alone and do not necessarily reflect the positions of my employers, co-workers, clients, family members or friends. This content is for informational purposes only and is not a substitute for medical or professional advice. Consult a qualified health care professional for personalized medical and professional advice.

