For many people, a continuum exists of feeling free and feeling trapped, of feeling free to _____ and feeling free from _____.
Confined to their homes, people may experience shifts along the feeling free/feeling trapped continuum. They may feel relieved from burdens, free to finish what they start, and trapped by circumstance.

When literally trapped by circumstance, people may find themselves up-close-and-personal with realities they have been able to avoid for awhile.
Note: “Avoidance” is a clinical term with judgmental overtones for the very human and humane desire to protect oneself from troubling feelings and thoughts. It’s not a moral shortcoming. It’s simply a practice that causes more problems than it solves in the long-term.
To help oneself with avoidance, one gently begins to approach uncomfortable realities with self-compassion and self-kindness.
People may feel backed into a corner in these areas:
- self: how they talk to themselves and treat themselves
- personal interaction style: the part they play in problematic patterns of interactions with others
- problematic interaction styles of others: what others do that cause problems in interactions and relationships
- mental illness symptoms: what thoughts, memories, and behaviors arise under stress
- avoidance methods: what they do to evade troubling feelings and thoughts when any of the above occurs
Self-concept example: People who repeatedly say to themselves, “I can’t handle this!” are going to feel terrorized by that belief because, in isolation, unless they have a 24-7 caregiver, they’re now the only person on the job.
Personal interaction style example: People who over-function in relationships and use the people they live with to reassure themselves are going to wear those people out. People who under-function and aren’t sustainably connected to the people in their worlds may find themselves losing energy and feeling disoriented from over-isolation.
Interaction style of others example: People who have tolerated disrespect, even cruelty, from their co-inhabitants, hoping things would work out or go away over time, may experience these frequently and painfully, perhaps in escalated form.
Mental illness symptom example: People who trusted they were successfully managing symptoms primarily through medications may find these symptoms “breaking through” the limits of assistance medication provides.
Avoidance method examples: Things people use and do to get away from all these challenges – alcohol, nicotine, marijuana, other drugs, overuse or underuse of food, overuse of the Internet, exercise, gambling, sex, the list goes on and on – may be in short supply, or no supply may exist, or they may be undoable because of lack of privacy.
You may be thinking: Whaaat?! I’ll have to look at all this all at once?!
Possibly.
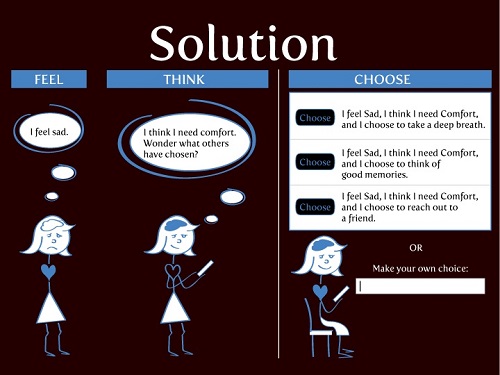
People may feel panic when they believe they are trapped. However, they can help themselves with panic.
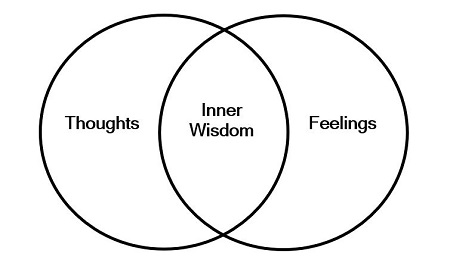
With an inner state in a more stable range, this process can be helpful:
“If I can become aware of the primary, natural feelings that arise, the thoughts I’m thinking, and the secondary feelings born of these thoughts, I can reassure myself and regain stability. I can sort facts from unhelpful beliefs, shift my attention to the facts, orient myself with my values and priorities, and help myself skillfully and effectively handle whatever is happening.”
Current crises are certainly on everyone’s minds and hearts. Whether in stable or unstable times, whatever is happening can call to us and we usually handle it as we’ve always handled it, sometimes unskillfully and ineffectually.
As never before, we are now called to be skillful and effectual.
Since addressing avoidance is a hard task, softness is needed. The task may be unwelcome and seem overwhelming. Separating the task into manageable parts may be helpful. Consider trying these questions:
What are the top two areas that may become problematic for me:
- in the ways I talk to myself and treat myself?
- in the ways I interact with others, particularly partners or my closest family member(s)?
- in the ways I have ended up being interacted with by others?
- in the ways I have managed mental illness symptoms (if I have them)?
- in the shortage or absence of what I often use or do to get away from what’s bothering me?
Even becoming aware of areas that may be challenging can offer strength to handle them. When problematic patterns arise, they are expected.
Simply recognizing when feelings are intense and thoughts are troubling can free people to pause and consider what to say or do next – or not say or not do – to be kind to themselves and others.
I theorize that gaining skill and power in the areas we have avoided will give us unprecedented skill and power to handle whatever happens in unprecedented times.
Wren West, L.P.C. contributed to this post.
Image: iStock
For people in the Blacksburg and Roanoke, Virginia areas who want to be able to follow up in-person after online counseling sessions, I recommend these providers of telehealth sessions: Stephanie Fearer, Ph.D., L.C.P. in Blacksburg (540-251-1567), and Wren West, L.P.C. in Roanoke (540-808-7948). I offer online counseling services to Blacksburg-area and Virginia residents as well, both individual and group sessions.
This guide to selecting an online counselor may be helpful.
The views expressed are mine alone and do not necessarily reflect the positions of my colleagues, clients, family members, or friends. This content is for informational purposes only and is not a substitute for medical or professional advice. Consult a qualified health care professional for personalized medical and professional advice.