“Addiction is bad people doing bad things.”
- “A substance use disorder is a medical illness characterized by clinically significant impairments in health, social function, and voluntary control over substance use.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 4-1 - “Addiction is a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences.”
– National Institute on Drug Abuse (NIDA), a division of the National Institutes of Health (NIH), 2014
“Addicts use drugs for pleasure.”
- 70% of people with substance use disorders have experienced trauma.
– Khoury et al., Substance use, childhood traumatic experience, and Posttraumatic Stress Disorder in an urban civilian population, Depression and Anxiety, 2010 - Half of people with substance use disorders have at least one co-occurring mental illness.
– Conway et al., Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions, Journal of Clinical Psychiatry, 2006
“Addiction is a choice.”
- Brain studies reveal that addiction compromises brain structures including the basal ganglia, extended amygdala, and prefrontal cortex.
– Nora D. Volkow, M.D., George F. Koob, Ph.D., and A. Thomas McLellan, Ph.D., Neurobiologic Advances from the Brain Disease Model of Addiction, New England Journal of Medicine, 2016 - “People suffering from addictions are not morally weak; they suffer a disease that has compromised something that the rest of us take for granted: the ability to exert will and follow through with it.”
– Nora Volkow, M.D., Can the Science of Addiction Help Reduce Stigma? Advances in Addiction & Recovery, Fall 2015
“Lock ’em up. That’ll serve ’em right. That’ll cure ’em.”
- The primary symptom of the illness of addiction is persistence in use despite negative consequences – including persistence despite the punishing, negative consequences of jail, prison, loss of custody of children, loss of one’s job, license to drive, license to practice a profession…
- For those with opioid addiction in the criminal justice population, maintenance medication can reduce rates of re-incarceration by 20% or more.
– Larney et al., Effect of prison-based opioid substitution treatment and post-release retention in treatment on risk of re-incarceration, Addiction, 2011 - Treatment is up to 7 times cheaper than incarceration.
– NIDA, “Is drug addiction treatment worth its costs?”, 2018
“Abstinence treats addiction.”
- “Remission of substance use and even full recovery can now be achieved if evidence based care is provided for adequate periods of time, by properly trained health care professionals, and augmented by supportive monitoring, RSS [recovery support services], and social services.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 1-19
“Abstinence from opioids treats opioid addiction.”
- 80% of people with opioid use disorder who try abstinence-based behavioral treatment or detoxification relapse.
– Gavin Bart, M.D., Maintenance Medication for Opiate Addiction: The Foundation of Recovery, Journal of Addictive Diseases, 2012
“People with addiction need to go to rehab.”
- Relapse rates when leaving rehab are as high as 70%.
– Laurel Sindewald, A Look at the Evidence for Addiction Rehab, our report, 2017 - More than half of U.S. rehabs use 12-step approaches.
– National Survey of Substance Abuse Treatment Services (N-SSATS): 2016 - Twelve-step approaches are not evidence-based as treatment for addiction.
– Laurel Sindewald, AA Is Not Evidence-Based Treatment, The Fix, 2017, updated here. - Most patients in rehab spend most of their time in group therapy.
“[D]espite decades of research, it cannot be concluded that general group counseling is reliably effective in reducing substance use or related problems.”
– Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs and Health, November, 2016, Page 4-26
“Drugs cause addiction.”
- 70-80% of people who try alcohol and other drugs do not become addicted to them.
– Maia Szalavitz, Genetics: No more addictive personality, Nature, 2015
“Big Pharma and prescription pain pills are to blame for the opioid crisis.”
- Less than 8% of people exposed to prescription pain medications become addicted to them.
– Nora D. Volkow, M.D., and A. Thomas McLellan, Ph.D., Opioid Abuse in Chronic Pain – Misconceptions and Mitigation Strategies, New England Journal of Medicine, March 2016 - Of 63,000 drug overdose deaths in 2016, fewer than 9400 involved prescription opioids, i.e. natural/synthetic opioids, excluding heroin/fentanyl.
– Drug Overdose Deaths in the United States, 1999–2016, Centers for Disease Control, December 2017
“Doctors are to blame for the opioid crisis.”
- 75% of people with pain pill problems received the pills from friends and family members, not doctors.
– Results from the 2014 National Survey on Drug Use and Health, 2015 - 70% of pain patients who developed opioid use disorder had a prior history of psychoactive drug use.
– Cicero et al., Psychoactive substance use prior to the development of iatrogenic opioid abuse: A descriptive analysis of treatment-seeking opioid abusers, Addictive Behavior, 2017
“Prescription pain pills are a gateway to heroin addiction.”
- Only 3.6 percent of people who misuse prescription opioids try heroin.
– Muhuri et al., Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States, CBHSQ Data Review, 2013, reported here.
“Overdose deaths are skyrocketing.”
- The spike in opioid-related deaths is presumed to be caused, not by prescription pain pills, but by inadvertent overdose through street supplies of heroin poisoned with illegally-made fentanyl and its analogues.
– Opioid Data Analysis, Centers for Disease Control, 2017
“If we declare war on opioids, we’ll solve the opioid problem.”
- Most opioid misusers also misuse other substances.
– Richard F. Catalano, et al., Is Nonmedical Prescription Opiate Use a Unique Form of Illicit Drug Use?, Addictive Behavior, 2011
– Soyka et al., Six-Year Outcome of Opioid Maintenance Treatment in Heroin-Dependent Patients:Results from a Naturalistic Study in a Nationally Representative Sample, European Addiction Research, 2017 - Most overdose deaths involve more than one drug. 97% of overdose deaths in NYC in 2016 involved more than one drug. UPDATE 2/21/18: Please read Maia Szalavitz’s report on substance combinations here.
– Health Department Releases 2016 Drug Overdose Death Data in New York City, NYC Health, 2017 - Anyone can get anything through the Internet.
– Olga Khazan, The Surprising Ease of Buying Fentanyl Online, The Atlantic, 2018
“Medication trades one addiction for another. Because methadone and buprenorphine are opioids, giving them to opioid ‘addicts’ substitutes one addiction for another.”
- Dependence is not addiction. Needing a substance to not experience physical withdrawal symptoms is dependence. Persistence despite negative consequences defines addiction.
– Sarah Wakeman and Maia Szalavitz, Why taking drugs to treat addiction does not mean you’re ‘still addicted,’ Stat, 2017 - “A person on buprenorphine is not in withdrawal, not intoxicated, not craving, not seeking and, most importantly, is free to return to a normal life.”
– Alan Schwartzstein, M.D., A Right Way to Treat Opioid Addiction, AAFP Leader Voices, 2/8/18 - On-going, long-term maintenance on methadone or buprenorphine are the only two treatments currently known to reduce mortality from opioid addiction by 50 percent or more.
– Pierce et al., Impact of treatment for opioid dependence on fatal drug-related poisoning: a national cohort study in England, Addiction, 2015
– Sordo et al., Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies, British Medical Journal, 2017
“Babies are born addicted.”
- Dependence is not addiction.
- “[A]lthough newborns may display physiological symptoms of drug dependence, they are not addicted.”
– Joshua Sharfstein, M.D., Neonatal Abstinence Syndrome: Déjà Vu All Over Again?, The JAMA Forum, 2015
“Opioid addiction is the biggest problem facing America today.”
- Marijuana overdose deaths: 0 (Source)
- Terrorism-related deaths, U.S. citizens, overseas and domestic: 32 (2014: Source)
- Prescription opioid drug-related deaths: 16,000 (2015: Source)
- Opioid-related deaths: 35,000 (2015: Source)
- Gun-related deaths: 35,000 (2014: Source)
- Drug overdose deaths: 64,000 (Provisional, January 2017: Source)
- Alcohol-related deaths: 88,000 (2015: Source)
- Obesity-related deaths: 300,000 (Source)
- Tobacco-related deaths: 480,000 (Source)
Oh, wait. Breaking news. Not 70s heroin? Not 80s crack cocaine? Not 2010s opioids anymore? Meth again?
- “The scourge of crystal meth, with its exploding labs and ruinous effect on teeth and skin, has been all but forgotten amid national concern over the opioid crisis.”
– Frances Robles, Meth, the Forgotten Killer, Is Back. And It’s Everywhere, New York Times, February 13, 2018
Wait, not meth? Benzos?
- “It would be a tragedy if measures to target overprescribing and overuse of opioids diverted people from one class of life-threatening drugs to another.”
– Lembke et al., Our Other Prescription Drug Problem, New England Journal of Medicince, 2/22/18
“Deciding to use substances like tobacco, alcohol, marijuana or heroin
does not make people less human. It reflects the fact that they are
human.”
– Hakique Virani, M.D., People use drugs, get over it, CBC Radio-Canada, 2017
“The iron law of drug prohibition is that the more intense the law enforcement, the more potent the drugs will become.”
– Richard Cowan, National Review, 1986, Wikipedia
Last updated 3/8/18
Image: iStock
. . . . .
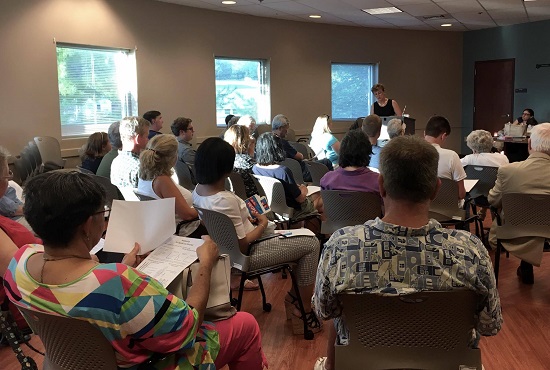
I will be giving a talk entitled “Opioid Epidemic? What Are the Facts?” for the Lifelong Learning Institute at Virginia Tech on Tuesday, March, 13, 2018, 3:15 – 4:30 PM, at Warm Hearth Village Center in Blacksburg, Virginia. The event is free and open to the public.
More information about the talk is here and here.
A follow-up discussion meeting will be held on Wednesday, April 25, 6:00 – 8:00 PM, in the Community Room at the Blacksburg Library, 200 Miller Street, Blacksburg, Virginia.
The views expressed are mine alone and do not necessarily reflect the positions of my employers, co-workers, clients, family members or friends. This content is for informational purposes only and is not a substitute for medical or professional advice. Consult a qualified health care professional for personalized medical and professional advice.