Robert “Bob” Hayes Giles, Jr., of Blacksburg, Virginia, 88, seeing he was too ill to be of further service to his family and others, died bravely on May 5, 2022 from voluntarily stopping eating and drinking (VSED). He suffered from neurodegenerative diseases resulting in symptoms commonly termed “dementia.” He donated his body to science to help researchers further understand these disabling disorders. He had no other illnesses.
Bob was preceded in death by his wife of 56 years, Mary Wilson Burnette Giles; his mother, Anna Rinsland Giles Trevey; his father, Robert Hayes Giles, Sr.; stepmother, Edith Lohr Giles; aunt Katherine Rinsland Irvin; grandmother, Lena Bosserman Rinsland, grandfather, George Herman Rinsland, father-in-law, Wilbert Glenn Burnette, and mother-in-law, Mary Thigpen Burnette. He is survived by his brother, George Giles and his wife, Lena, and their children and grandchildren; step-sister Susan Lohr Hudson; brother-in-law W. Gaines Burnette and his wife, Peggy, and their children, grandchildren, and great-grandchildren; cousins Kay Hughes and John Irvin; daughter, Anne Giles; daughter, Margaret Galecki; son-in-law Dennis Galecki; former sons-in-law Mark Wiley, Brad Rimbey, and Iain Clelland; grandson Alan Wiley, his wife, Mary “Woo” Wiley, their son, great-grandson Beau, and their daughter, great-granddaughter Dottie; grandson Ben Wiley; granddaughter Mary Teague and her husband, Chad, and their daughter, great-granddaughter Raine; grandson James Galecki and his wife, Renee, and their sons, great-grandsons Logan and Liam; granddaughter Caroline Galecki; and granddaughter Catherine Galecki.
Bob was born on May 25, 1933 in Lynchburg, Virginia. He attended E. C. Glass High School, during which he was awarded a Bausch and Lomb Science award for studies of the ring-necked pheasant. As an Eagle Scout, he was awarded the W.T. Hornaday National Award for Distinguished Service to Conservation and the James E. West Scouting Conservation Scholarship. During his undergraduate years at Virginia Tech, Bob was an editor for several magazines and the president of the V.P.I. Corps of Cadets of 6,000 students. He was also a member of seven national honorary societies.
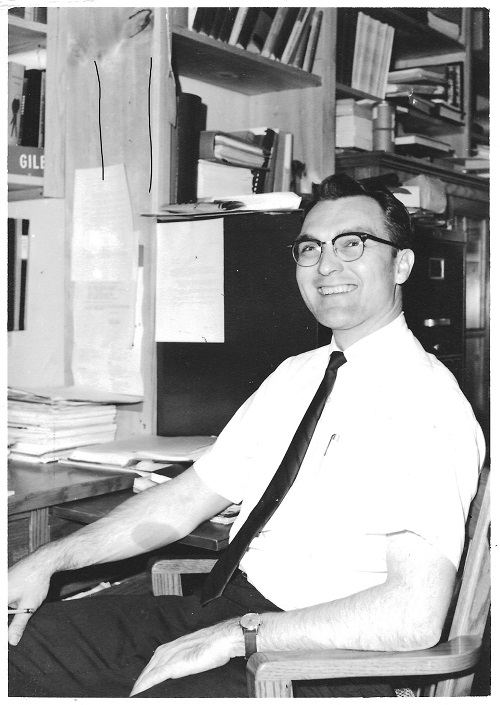
Bob was a Professor Emeritus of Wildlife Management at Virginia Tech where he taught for 30 years. His Bachelor of Science degree in Biology and Master of Science degree in Wildlife Management were from Virginia Tech. His Ph.D. in Zoology was from The Ohio State University. He was a recipient of The William E. Wine Award, given for a history of university teaching excellence.
In the early 1960s, Bob was a pioneer in envisioning use of computers for natural resource management. He and his graduate students meticulously recorded data about the land by hand, then used computer programs on decks of punched cards to analyze it. This process is now done through satellite imagery and is known widely as Geographic Information Systems (GIS). In 1968, he learned of general system theory and became a systems thinker. He believed that problems are interconnected and that a system of problems must be met with a system of solutions.
During his time as a professor in the Department of Fisheries and Wildlife at Virginia Tech, Bob was known for his innovative applications of computer programming. With the support of the Tennessee Valley Authority (TVA), he created the woodland resource management system of TVA, once used on 300 farms a year. With staff and students, he created the first wildlife information base (BOVA – Biota of Virginia database). He chaired the Blacksburg planning commission, consulted with the National Wildlife Refuge System, aided the State Cooperation Commission, and wrote the first plan for wildlife other-than-game for Virginia.
Bob was a speaker at the first Earth Day at Virginia Tech on April 22, 1970. When challenged by a student in the audience, “What are you doing about zero population growth, Dr. Giles?”, Bob held up his hand in a peace sign and answered, “Two children and a vasectomy!” He was unafraid of challenging taboos for the sake of others.
At his retirement party, colleague Larry Nielsen said, “Giles has more ideas in an hour than most people have in a lifetime.” When she was a teenager, his daughter Anne remembers her father asking what she wanted written on her tombstone. She returned the question. He answered: “He contributed to science.” Bob lamented hearing often that his ideas were “great” but “ahead of their time.” Recently, a former student remembered thinking in the 1970s that Dr. Giles’s ideas were “out there.” He said, “They’re now standard practice.”
Bob began working on the concept he termed “Rural System” in the early 1980s, and in earnest after his retirement in 1998. He envisioned Rural System as a GIS-informed enterprise to improve the social, economic, and environmental health of regions through optimal use of resources via a system of for-profit, citizen-owned entities of multiple, small, natural resource-related enterprises. He was aided in completing his final research work by Risa Pesapane, now a Ph.D. and professor at The Ohio State University, and Laurel Sindewald, now a Ph.D. candidate at the University of Colorado, Denver. His final work, “Rural Future: An Alternative for Society Before 2050 A.D.,” was edited by Laurel Sindewald.
Raised in Southwest Virginia, Bob knew the struggles of people in Central Appalachia, impoverished after the collapse of the coal and tobacco industries. To further his knowledge, after retirement, he visited rural areas of Africa – Nigeria, Senegal, and Uganda – China, and India.
Bob was friends for nearly half a century with Airport Acres neighbors Mills and Betty Jo Everett, and Bill and Lois Patterson. During his final years living at his beloved house on Rose Avenue, Bob recounted with laughter and wonder his local adventures with friend Caleb Flood.
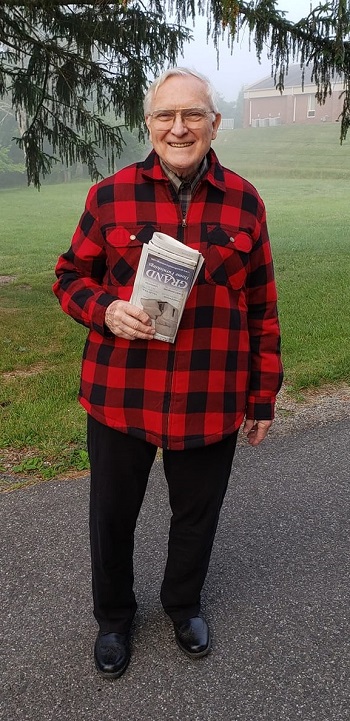
Bob spent the last years of his life at The Heritage House with two other residents under the care of Hugh Bowman and his staff. Bob considered Hugh a friend. Perceiving his fellow residents to be treasured graduate students, he read the newspaper to them and tended them as he could. Bob’s family thanks Hugh and Kim Bowman, devoted members of the staff at The Heritage House, Andrea Hendricks, Clidia Lewis, Kathy Merideth, and kind companion Jo Burks, for the gentle, respectful, well-tended days they gave him. Bob’s family thanks Dr. Gregory Beato for his compassionate medical care.
Bob was known for his ability to look realistically at problems, but to see vast systems of solutions in radical, unprecedented ways. He championed science, facts, reason, logic, and humanity. He could be counted on for principled living, courtesy, and kindness. Some considered him valiant, noble, and saintly. Bob mentored and corresponded with former graduate students into their own retirements. To the last, he grieved the loss of his understanding and lamented being unable to protect his daughters from the hardships of his illness and these times. Before he lost the ability to articulate his thoughts, however, Bob said, “It’s been a grand adventure.” With nearly all of his brain function gone, unable to speak and barely able to move, within hours of the end of his life, he found the wherewithal to smile at his daughters.
As to his legacy, as former graduate student Bharat Bhushan, now a professor in India put it, “I only know, even as I am so far away, that his mind reaches out to me and many others, and talks to us. I was, am, his student, forever.”
Bob often signed his letters, then his emails: “Pax.”
In memoriam, when you open the next door for someone or bring in your neighbor’s bins from the curb, please think of Bob Giles.
A visitation with family members will take place on Tuesday, May 31, 4:00 – 6:00 PM, at McCoy Funeral Home in Blacksburg, Virginia, U.S.A.
To honor Bob’s life and work, you are invited to contribute to the Robert H. Giles, Jr. Scholarship at Virginia Tech, Virginia Tech Foundation, 902 Prices Fork Road, Blacksburg, VA 24061.
The biography and CV of Robert “Bob” H. Giles, Jr. were last updated by him in 2018. They originally appeared on his website, “Rural System.” At the end of his working life, he self-published Rural Future: An Alternative for Society Before 2050 AD, edited by Laurel Sindewald. His daughter, Anne, wrote a tribute to him, Letter from the Universe, in March, 2022.
“Meanwhile, the gratitude I’ll have this Thanksgiving will still come: from having had the chance to know this love, even in its pain.”
– Sarah Wildman, writing about her daughter, 11/19/2023