Although this page is public, it is intended for the former graduate students, colleagues, family members, and friends of Robert H. Giles, Jr., who valued his thinking.
My sister and I expected to describe our father’s death using words similar to Brian McGilloway’s about his father: “He left this life as he had lived it, gently, quietly, without fuss, surrounded by family and prayer, knowing he was loved beyond measure.”
Instead, we witnessed our father’s needless suffering.
Below is a potentially alarming and distressing chronicle of our father’s final years. I believe it tells a cautionary tale for all of us.
This portion of this page is a neutral summary. Below, beneath the horizontal line, begins the strongly-worded portion.
Science tells us to approach reality and examine it closely; humanity tells us some realities must be approached slowly, at the right time, or not at all. Assess your needs and wants and trust your inner wisdom about whether or not to read beyond the demarcation.
We share the story of our father’s last years for many reasons.
Our father, quoting Socrates, said, “The unexamined life is not worth living.”
We believe that, if our father could have spoken, he would have spoken up and spoken out. What happened to him is tragically common and is likely to become more so. We believe he would urgently caution you to do the best you can to protect yourself, your loved ones, and fellow humans from the current state of end-of-life care.
I believe I engaged in scholarship as my father would have and conducted meticulous literature reviews of the research on the nature and treatment of the neurodegenerative brain diseases that cause the set of symptoms termed “dementia.” I report and distill many of my findings here. I conclude that, currently, protective personal actions one might take are:
- Consult an attorney and write the most specific and comprehensive advance medical directive allowed in your state or nation.
- Write a detailed, specific advance directive for dementia care. Consult an attorney and attach as much legal power to it as possible, including signed and dated signatures of witnesses. Although supplemental advance directives may not be legally honored in your locale, expressly stating your wishes gives those responsible for your care the power to advocate on your behalf, able to cite your documented, witnessed words to corroborate their efforts. Although entitled “my advance directive,” between the lines of this research-informed advance directive for dementia care that I have compiled and published for all to use in consultation with a legal professional is the story of the indignities and injustices endured by my father.
- Support your representatives’ attempts to pass death with dignity laws at state and national levels.
Although our father didn’t die peacefully, in our view, he died heroically. Further, of only one or two per year from our locale who donate their bodies for anatomical study, even unto death, he was braver than many.
On March 5, 2022, one of dozens of times she went with me to see my father, Virginia Tech visiting scholar Tian Gan, Ph.D., sat next to me on the floor. She whispered in my ear, “May I take a picture?” I nodded. Below is the photo she took, which I have her permission to share, two months before my father died.
My father said, “Love unto death.”
It was my honor to be his daughter and to love and care for him.
Robert H. Giles, Jr. Professor Emeritus of Virginia Tech, revered professor and beloved father, died May 5, 2022. Here is his curriculum vitae and here is his obituary. At the end of his working life, he self-published Rural Future: An Alternative for Society Before 2050 AD, edited by Laurel Sindewald. I wrote a tribute to him, Letter from the Universe, in March, 2022. He donated his body to science.
. . . . .
. . . . .
I, Anne Giles, eldest daughter of Robert H. Giles, Jr., have debated long and hard about how and why to share the story of his last years. They were an anomaly. He was unable to speak about them. He was the kindest of men. He was also a hard-hitting, relentless scholar. He protested injustice. He asked me to share any parts of his story that might be helpful to others. He asked me to be his voice.
“Don’t play small,” my father said.
When asked at the first Earth Day what he was doing about zero population growth, he believed the world needed to know he had two children and a vasectomy. He was fearless about sharing his personal life in hopes of helping the lives of others.
So be it.
The following is my imagined transcript of his last lecture, the day after his death. Most of the links are to posts I have written about his situation over the past year.
I know it is also a wail of mourning and imagined words of guidance and comfort from him.
My father was silenced by undiagnosed neurodegenerative brain disorders that resulted in the symptoms known as “dementia.” He attempted to speak, but the words were out of order, then became unintelligible. Towards the end, my sister and I sat close to my father, leaning towards him, all of our faces inches apart, alight with simply being together. Trying hard to focus his eyes on us, the last clear word he uttered to me and my sister was, “Wonderful.”
With no other illnesses and longevity on both sides of his family, he expected to live to 100, writing articles, corresponding with graduate students, and gardening into his old age. Should he become frail, “Put me in an old folks’ home and forget me!”, he told me and my sister. He refused to live with us, not wanting to burden us with elder caregiving, having witnessed as a child his young mother struggle to care for two little boys and her husband’s elderly aunt. My father led a circumscribed life, serving devotedly and without complaint as my mother’s primary caregiver for decades, then his mother’s care coordinator. “Be free!” he said. “Live your lives!”
What none of us planned for was my father to lose his greatest gifts to the world: the ability to remember what he knew, to use logic and reason to draw conclusions and make decisions, to voice his own wishes with his brilliant words. We didn’t plan for his keen ability to read data to become filtered through a perception skewed by dementia-related psychosis. His new data set came from hallucination, seeing and hearing things that others did not; his new hypotheses were based on delusion, holding beliefs that were not true.
At his first assisted living facility, before this Professor Emeritus was evicted, which “he” will explain below, my father sorted papers from his filing cabinets. He handed me a piece of paper, first dated 1996, with these typed words:
“To whom it may concern…or to anyone who will read this. If I get Alzheimer’s disease or related diseases or disability, I need to die as soon as possible. I want this to occur. I want assistance in any and all ways possible that will not endanger family or friends or jeopardize them for court action. I want to donate body parts, as many as possible, and that are suitable, given my final condition, to hospitals or university anatomical/pathology units. I’m writing what is my desire now since I believe that when I am in the last stages of illness I cannot decide anything. I need help in stopping my life when the appropriate time comes. Hard to know when such time has come, I believe it will be when any 3 people who know me think (expressed by their expert judgement) that I am operating mentally at less than 70% of my normal mental function.”
Once again, my father’s ideas were ahead of their time.
From this data and more, I hypothesize what my father might say the day after he died. On May 12, 2022, as I write this, by 9:00 PM tonight, he will have been gone one week.
The content will be an imperfect guess. Even with dementia, with me in my 60s, my father asked, “How about a Ph.D.?” I never did get that Ph.D., so the depth of my understanding and expertise is limited. I have tried not to misrepresent his ideas, but I may have.
I do my best to express his views. They are not necessarily mine. I have many of the same views as those of my father as I have expressed them, some stronger, weaker, and different. I have done my best to tell his story, not mine. The content is speculative and subjective, of course, not objective. I did, desperately, want to ask him what he was thinking and feeling, what he would say. Until my own end, I will.
It’s presumptuous to assume even a daughter would know what Dr. Giles might feel and think in any circumstances, much less with the privations he endured. After doing a cost-benefit analysis, I assessed the potential benefits of speaking up, perhaps imperfectly, as outweighing the potential costs – even the dire costs – of silence.
I do trust my vocabulary. I was taught words and ideas by him – “epistemology” at 13, “cost-benefit analysis with rank ordering” at 16 (to decide whether or not to stay with a boyfriend!), “optimize within constraints” at 60.
As a trained counselor, I’m adept at empathy. I’m a good student and can recall a good teacher’s lecture. While I was an undergraduate at Virginia Tech, I took my father’s Principles of Wildlife Management course and I have read his textbook, cover to cover. I earned that A.
So I will try.
My hypothesis is that any of his graduate students could also have written this lecture. My father was unambiguous in his views about mercy and humanity.
I am imagining him at a podium, in an auditorium filled with his beloved graduate students and colleagues. This text is just under 5,000 words, deliverable in about 50 minutes. In his customary suit and tie, I see him restored to clarity, speaking strongly into the microphone, making intent eye contact with us, giving us his final words.
. . . . .
“How did we get here?!”
This is the question I asked my daughters outside the locked assisted living facility we had just toured.
Let me provide some context. In 2016, I gathered with my daughters at my attorney’s office and signed documents leaving all of my possessions to them equally. I stated my wishes in case I became ill, including my request to be put in an assisted living facility if I became a danger to others. I signed an advance medical directive stating I wanted no medical treatment in case I became terminally ill, and powers of attorney. My daughters’ names were added to all my accounts. With those documents and my actions, my daughters could have written checks for their own purposes, had me declared mentally incompetent, and taken everything I owned. I have boundless love for, and trust in, my daughters.
When my daughters told me it was time to move into an assisted living facility, with profound sorrow, I complied. They were following my wishes. In August of 2018, I left the beloved home I had shared with my beloved wife, and moved into a pleasant-enough apartment at a forward-thinking assisted living facility founded by Virginia Tech colleagues.
In the next room that served as my office, I told my eldest daughter I heard people speaking. In the chair in my living room, I described to her a man who sat silently. My wallet went missing. I began hiding my possessions from thieves. I tried to call my daughters but I had forgotten how to use the phone, even when their photos were pasted to the touch buttons. I began leaving my apartment at night to escape the silent man and to look through the residence’s industrial kitchen for associates of the people in my office. I was escorted back to my room, but I didn’t believe the staff member’s reassurances that I was safe. I could hear the voices. I could see the man.
Late on a winter night, I had had enough. I put on my hat, grabbed a length of the 2″ x 4″ I used to protect the rug from my toolbox, walked out the facility’s side door into the snow, and headed down the road to my friend and assistant’s house, about two miles away.
I was nearly there when the facility’s van pulled up beside me and insisted I get in. I complied. I was returned to my room with the people in the next room and the silent man in the chair.
When I heard my eldest daughter’s voice at the door, I cried out, “Save yourself! Run! It isn’t safe!” Only when she begged and begged did I let her in. I am not proud of this, but for the first time in my life, I sobbed in terror and despair in another person’s arms.
When my childless, eldest daughter adopted a cat in 2002, my wife and I drove to Tampa to support her. When we had a moment alone, I said, “Pets bring joy and pets bring sorrow. I know this is a difficult subject, but this cat is helplessly dependent upon you. If it gets injured, it needs to die as soon as possible. This is how you do that.” And I taught my daughter how to quickly euthanize her own cat. Mercy must triumph over societal expectations and taboos.
My flight from the facility on February 3, 2019 was where my story should have ended. I had developed terminal illnesses that were injuring my brain, symptoms defined by dementia. These symptoms would progressively worsen, for which there was no treatment and no cure. My quality of life was nearly zero. My actions had become irrational and potentially dangerous. My mental, emotional, and existential torment were acute. I had caused agony to my daughters. I had utilized health care resources beyond my lot for incurable illnesses rather than for health. Simply put, as a result of irremediable sickness, I had become a malfunctioning organism. I needed to be euthanized as quickly and mercifully as possible.
As I stated in the document that supplements my advance directive, under these circumstances, it was my wish to die.
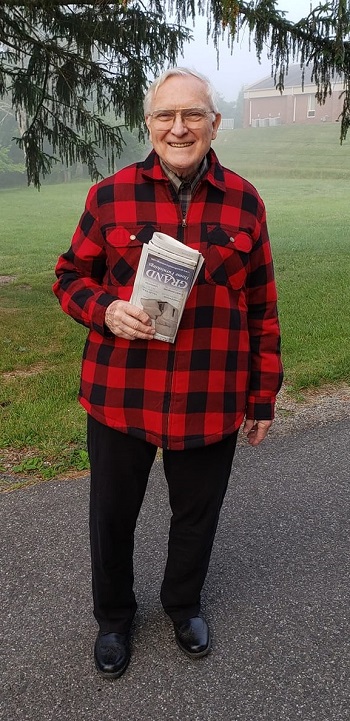
I acknowledge how anguish-filled this is for all involved. Look at my face in this photo, taken of me by my eldest daughter about two weeks after my first break with reality. I see my delight in her. I see a shadow of distress as well. I’m not myself. There’s an artificial intelligence app from Australia that reads facial microexpressions to assess pain. I wonder if it can be used on photos. I wonder what its report would be.
As hard as this may be to hear, even though I love my daughters deeply, if I am not myself, I would rather not live.
But these discussions are irrelevant. If my wishes, stated in my supplemental advance directive in case I developed dementia, had been honored, the need for these agonizing debates would have been non-existent.
My physician should have been able to prescribe a lethal dose of a medication. As author Amy Bloom did for her husband when he received a dementia diagnosis, accompanied by my daughters, perhaps with a glass of scotch on the rocks, I should have been allowed to swallow the medication and, with enough of my heart and mind intact, feel a final swelling of love for my life, for my wife, my parents, my grandparents and my brother, for my extended family, for my students and colleagues. for the people who have touched my life – for, truly, all of humanity – and for my dear, dear daughters. I could have passed sadly but peacefully, safely, and quietly in their loving company.
Instead, what began was a three-year and three month saga of alternating suffering, horror, and boredom. I was evicted from the first facility as a “flight risk,” was not put into the locked facility, but placed in a small, private care residence. The caregivers were attentive and the residents were well-tended. With them, I ate, shat, and watched television, often “The Golden Girls,” “Gunsmoke,” and interminable Christian programs.
“Just a minute!” my wife called out to my eldest daughter, then in her teens, who came home unexpectedly to find the front door of our Airport Acres home locked. I treasured my intimate life with my wife, my one and only sexual partner. I disrobed only for her. I began to not remember how to tie a tie. Clothes became anathema to me, especially shoes and socks. During my last year, strangers viewed and bathed every single part of my body.
Each day, I hesitated, but asked my daughter if my wife, Mary Wilson, might visit today. Every day, she bravely controlled her face and said she was so sorry but my wife, her mother, was gone. Every day, I felt the shock and sorrow of losing my wife anew. Each night, I paced my room, looking everywhere for what was lost. Every morning, I awoke aching with aloneness, wondering why I had been left at this strange place with these strangers. Tentatively, I went through my beloved people. Might my mother visit today? My grandparents? My daughters?
I asked the lady who came to visit every day, “Have you seen Anne lately? Might she come to visit?” My eldest daughter tried to control her face. She said, “I am Anne. I am here for you.” I apologized profusely.
I tried to control my own face when I peered through the windows and saw threatening men and animals outside. I didn’t want to alarm the other residents. I picked up furniture, weighing it to hurl at invaders. Inside, strewn on the floor, I saw dismembered animals and people, tiny children needing saving in the midst of the carnage. I reached out to them, over and over. I asked aloud, “Are you all right?” Lost and bereft, I admit I told my daughter what I saw. I regret this. I fear these visions haunt her, too.
I developed friendships of sorts with the residents. In the course of those three years and three months, I gained and lost and grieved six friends – one a treasured colleague from my previous life – witnessing their declines unto death.
How often did I hold back tears?
Then I began to see some kind of particulate matter on the floor that needed careful collecting. I spent many hours of many days of many months bent on my hands and knees with my 88-year-old body, gathering the particles. I grew callouses on my fingertips. When urged to stand, I fought off my caregivers. This needed to be done. My eldest daughter dropped to the floor with me. Sometimes I would stream handfuls of the matter into her hand as if it were glitter. A few times she asked, “Is this soil? Is this a garden?” I would nod. But I wasn’t sure.
I was started and stopped on probably a dozen anti-psychotic and anti-anxiety medications, all to no avail. There’s no medication to stop a brain from rotting like a bad peach. There’s no anti-anxiety meds for the existential horror of witnessing your own personhood decay before your very eyes. Might the meds have helped ease my distress? I can’t say. But they ricocheted through my personhood like rockets.
Whatever the medications did, it wasn’t enough. My eldest daughter’s phone is full of photos of me suffering – on the floor, with my face in grimaces and frowns, in abject sorrow. She forwarded them to all the powers-that-be, advocating fiercely and tirelessly – to the point of being patronized, reprimanded and threatened right before me, with me speechless and wordless to protect her – for me to receive enough effective medications, at high enough doses, with enough frequency, to have some semblance of ease. Shame is the primary feeling of people who care for people with dementia.
At a euphemistically termed “team meeting,” I heard the hegemonists of the health care system speak about my case. My daughters listened silently, helplessly. With the last tatters of my personhood, with my own metaphorical 2″ x 4″, I again took matters into my own hands.
By law and policy, caregivers are required to feed me. I had to fight the “rooting reflex,” the broken adult brain’s instinctual opening of the mouth when a spoon is touched to it. In order not to swallow the food put into my mouth, I had to let it dribble from my lips onto the front of my dress shirt. I was repelled by this but saw no other way to achieve my objective: to save my daughters from further suffering by euthanizing myself through the only means left to me – starvation and dehydration.
Why didn’t I do this earlier? Was I indecisive?
While in the U.S. Army Rangers, I applied for a leadership position. At the interview I was told, “Giles, you’re indecisive. Leadership requires someone who can make a decision quickly and take action.” Perhaps I seemed indecisive in those circumstances. I see a universe of possibilities in every moment! I pause in wonder! Then I analyze. Then I decide.
I believe instinctual portions of my brain still worked. The parental bond is brain-deep. With my increasingly unfocused eyes, I saw my worried, beleaguered daughters. I stayed for them. When I observed my staying was causing more unintended harm to them than my intended good, I was able to gather what was left of myself together. I was decisive.
Medications I had been given by pill and mixed with food, I was no longer able to receive when I stopped eating and drinking. Liquid forms needed to be researched, compounded, gotten over the weekend, perhaps by Monday or Tuesday, la-la-la. Unable to speak or move, withdrawal symptoms coursed through my heart, mind, nervous system, and body.
With caregivers’ reluctance and disapproval, I was given pain medications, in low doses, not based on my distress, but on a set schedule.
I did not die peacefully. My end-of-life managed by a belief-incarcerated, ascientific system, I died in withdrawal from old medications, insufficiently dosed with new medications, emaciated and dehydrated, gasping for air.
I see this as three years and three months of meaninglessness, of no utility whatsoever. It was wasted time, wasted human resources, wasted material and financial resources, and nearly unbearable, needless suffering for my family.
Why am I telling you this story of woe?
As I did to my daughter, I cry out to you, “Save yourself!” I add, “Save the beloved people in your life!” And, “Save others if you can!”
This never should have happened. It should not have been allowed.
But everyone was following law and policy.
“How did we get here?!”
Horrifically and tragically, what happened to me is common. It will become increasingly common since occurrences of dementia are expected to increase.
What’s to be done?
How can we transform this? It is so complex. There are so many variables…
What could I have done differently? What is my part? Was I indecisive when I realized my mind was slipping? Should I have taken my own life while I still had my wits about me? How, legally, without traumatizing my daughters? I remember telling my eldest daughter, “My brain is scrambled.” Instead, long ago, I think, unknowingly and unwittingly, I made two errors in logic.
First, I assumed the social contract and universal humanity would respect my wishes and care for me in old age. How a society treats its most vulnerable citizens is a measure of its goodness. I believe we are, at essence, good.
Second, I assumed people would follow science. Science is use of the best aspects of the best human minds to describe reality as we can understand it today. Why wouldn’t I be able to trust us to develop reality-based strategies and follow reality-based policies?
Looking back, I see I did not – and did not teach my graduate students to do this – describe the findings of research for the general public. I admit to arrogance, to believing that people should aspire to learning how to read scientific papers. I neglected my responsibility to help laypeople understand in words they could understand. This has had tragic, dreadful consequences. I profoundly regret my part in this.
What are the solutions?
Support passage of “death with dignity” laws. The social contract is supported by laws. If I had lived in a state or nation with death with dignity laws, this story would have ended with sorrow and love, not suffering and love. I see in my state that progress has stalled with a tie vote in a committee. I testified as an expert witness before Congress to oppose construction of the Gathright Dam. I regret forgetting that humans need laws, informed by expertise, to help them live well together. I should have helped my state’s representatives pass death with dignity laws.
Write specific advance directives for dementia care. I know better than to not define terms! I should have specified everything of value to me. For example, I should have stated that I consider “spoon feeding” to be “artificial feeding.” If I can’t naturally feed myself, then I consider any other means artificial. I should have defined “pain.” I should have defined “suffering.” My eldest daughter has compiled a research-informed advance directive for dementia care based on my bitter, hard-won experience. Perhaps it can be adapted for your own purposes. She is not a legal professional. Seek legal expertise! Perhaps you can prevent yourself and your loved ones from experiencing the indignities, injustices, and suffering I endured.
I can imagine hearers of this story might exclaim, “What an ignoble end!”
Not so.
I champion love and life. I champion knowledge. I serve the greater good, even when conventions and niceties are preferred.
Although I witnessed the debate but couldn’t contribute, my daughters and caregivers considered whether or not I should have a COVID vaccine, given that I requested no medical care. In hopes of protecting other residents and staff from infection, it was decided I should have the vaccine. Silently, I concurred.
Only one or two people from my locale, per year, donate their bodies for anatomical study and surgery practice to our state’s universities and research facilities. In this nation, once upon a time, only the bodies of executed criminals could be dissected. I defy this ascientific taboo.
My eldest daughter has penned this missive from her memory and imagination. After death, I believe I have no sentience. I am an arrangement of hydrogen, oxygen, carbon and nitrogen, no more, no less.
Foregoing the conventions of cremation or burial (the latter a waste of land resources, I have declared a hundred times), I donated my body to the Commonwealth of Virginia, the grantor of my pay check and retirement income since 1968.
If I had not had a COVID vaccine, my body would have been rejected.
In his latest memoir, psychiatrist Irvin Yalom describes, as a medical student, taking a break with fellow students from dissecting their assigned body, an older gent, to play bridge next to the cadaver.
I am at a university! As was always my greatest wish, in spite of everything, even in death, I am contributing to science. Exult with me!
Ut Prosim.
The medical students using my body to learn and grow are probably taking a break to use their mobile phones. I hope they are leaning their elbows comfortably on my old shoulder, messaging their loved ones of their hopes and dreams.
Did I know any of what my eldest daughter has described here? It’s hard to say. I concur with Freter that we cannot validly draw conclusions about the inner state of a person with dementia.
Yet, a day or two before I died, when my forlorn, eldest daughter laid her head on my skeletal chest for comfort, I used every ounce of my strength to lift the claw that had become my hand to stroke her hair. Did I know who I was or who she was? I’m not sure. But I know what love is. It lasts and it matters.
Don’t fret. Be comforted. It’s over. If you saw me in the last few years and have troubling memories, don’t give them a second thought. They mean nothing about you, my regard for you, or about my life and work.
Live. Love. Be free. Be brave. Don’t turn away – not from reality, not from the person lying defenselessly by the side of the road. Follow knowledge. Serve the greater good.
Pax.
. . . . .
Robert H. Giles, Jr., Professor Emeritus of Virginia Tech, revered professor and beloved father, died May 5, 2022. Here is his CV and here is his obituary. At the end of his working life, he self-published Rural Future: An Alternative for Society Before 2050 AD, edited by Laurel Sindewald. I wrote a tribute to him, Letter from the Universe, in March, 2022. He donated his body to science.
This content is for informational purposes only and is not a substitute for medical, professional, or legal advice. Consult qualified professional for personalized health care, medical, legal, and professional advice.